Do you know 68% of marketers use a form to maintain lead scores as the leads move through the funnel? With marketing automation, gone is the need to maintain such kind of forms. Automating the lead scoring process gives you intelligent insights into the leads to persuade at first.
This lead scoring guide demystifies the nitty-gritty details of how to score a lead before finding the right ones to engage with. Here is a sneak peek into what you will be reading:
Are your sales team member running after the right lead?
Are you making the process easier so that your sales team actually gets leads that they can sell to?
Are you pursuing leads who have a high purchase intent?
Can you segregate marketing qualified leads (MQL) from sales qualified leads (SQL)?
Are you able to track the sources that are giving you some of the most valuable leads?
Lead scoring has an answer to all these questions. It takes the demographic and behavioral information into account for awarding points to prospects.
Understanding lead scoring meaning helps you to focus on the right prospects who already have shown a great deal of interest in your product.
Do you know 68% of marketers use a form to maintain lead scores as the leads move through the funnel? With marketing automation, gone is the need to maintain such kind of forms.
Automating the lead scoring process gives you intelligent insights into the leads to persuade at first.
This lead scoring guide demystifies the nitty-gritty details of how to score a lead before finding the right ones to engage with.
Here is a sneak peek into what you will be reading:
- Lead Scoring Definition
- What Are the Different Lead Scoring Models?
- 5 Behavioral Traits to Include in Lead Scoring Process
- 3 Lead Scoring Techniques for Calculating Lead Score
- 4 Benefits of Implementing A Lead Scoring Strategy
Lead Scoring Definition
The process of lead scoring does exactly what it says. Lead scoring is a method to measure the value of prospects. The value of a lead determines on its engagement in various activities such as visiting the web page, submitting an inquiry, receiving a sales demo, etc.
This quantitative element helps your sales team to prioritize leads that are likely to convert. An efficient lead management system lets you score your leads so that you get to understand who is really interested in your product.
A higher lead score translates into increased chances of a lead getting converted.
What Are the Different Lead Scoring Models?
A lead scoring model remains at the core of the entire process of lead scoring. It determines the attributes based on which a lead will be evaluated.
Depending on your business, you can adopt a lead scoring model below. However, these models function depending on what kind of data you are able to collect. Here are the six widely used lead scoring models:
a) Online Behavior: A lead’s online behavior can speak about his or her interests to a great extent. Online behavior refers to the way in which a lead interacts with your website. For example, a lead might visit the pricing page 3 times a day. Such activities should ideally contribute to a high lead score. While measuring online behavior, here are some of the attributes to score a lead on:
1) Resources downloaded
2) Pages visited
3) Forms filled
4) Offers availed
b) Business Specific Information: Has it ever happened that your sales team called a lead only to know that your product isn’t fit for the lead’s industry?
Well, there is a way to know that before making the call. Once you put fields such as company size, type, and industry on your landing page, you will be able to award a higher score for those who fit with your target group.

c) Demographic Information: Your lead scoring model can be based on demographic information as well. This will help you to eliminate leads located outside the geographic area you serve.
Adding different fields i.e. zip code, city, state, country in your landing page becomes much easier when you adhere to the landing page best practices. This lead scoring model example will assist you in prioritizing leads coming through inbound marketing.

d) Social Engagement Metrics: Your lead scoring model can combine social engagement metrics as well. If your target buyer persona is on social media, you definitely need to track their engagement with your content.
For example, consider the number of retweets of your post or click-through rate on your LinkedIn post. This will help you to award points to those who engage with you on social media channels.
e) Detecting Spam: Since the entire idea is to prioritize leads, you should focus on detecting spam as well. For example, you can award more points to those who use a business email address while filling a form on your website.
You can also filter leads based on valid information entered in different fields of a form.
f) Email Engagement Metrics: You definitely don’t want to miss those leads who always open your emails. This is why it is important to award more points to those who do.
As you track email metrics, you will be able to know the leads who opened promotional or nurturing emails. This enables you to segregate the leads even better.
If you operate a small business, here is a freebie for you: Best email marketing practices for small businesses.

5 Behavioral Traits to Include in Lead Scoring Process
With all these lead scoring models mentioned above, now you must be thinking how to combine all of these to configure the best lead scoring rules. Well, building a relevant lead scoring system doesn’t have to be difficult. Here are 5 behavioral traits that you can combine to create the perfect lead scoring system:
i) On-page Search: Tracking on-page search queries gives you a better idea about what your audience is interested in learning. For example, if a lead searches for pricing options, you should definitely assign a high score to that lead.
ii) Downloads: When a lead visits your resource page to download a white paper or case study, chances are high that they are looking forward to have a problem solved. You should definitely award them with a high score.

iii) Page Views: A lead will not visit your website multiple times on a day unless they are really looking forward to a solution for the challenge they are facing. If they are visiting high-value pages such as the pricing page, you should ideally assign them a high score.
iv) Email Open Rate: Email open rate should be a significant lead scoring criterion for you. When a lead opens your email, you know they are interested in your product.

v) Webinars: Are your leads attending your webinar? If they have chances are high that they are willing to know more about your product. That’s why you should award them with a high score.
3 Lead Scoring Techniques for Calculating Lead Score
Calculating a basic lead score is not that tough with a lead management system in place. There are 3 techniques using which you can calculate the lead score at ease:
1) Manual Lead Scoring: Manual lead scoring is time-intensive and difficult to do when you have thousands of leads flowing in. Here is how you can calculate manual lead scoring:
Get the lead-to-customer conversion rate by dividing the total number of customers by the total number of leads generated.
Choose the attributes that you believe high-quality leads had.
Figure out the close rate for each of those attributes.
Compare the close rates of these individual attributes with the overall close rate.

2) Data Mining Lead Scoring: Data mining lead scoring uses mathematical techniques such as logistic regression. In this method, a formula tells you the chances of a lead converting into a customer. Using these techniques of survival analysis for scoring leads will help you to have an exact figure.
3) Predictive Lead Scoring: The best lead scoring solutions are using predictive lead scoring to analyze data to understand the common points shared by those leads which converted. In addition, this applies the same formula to find potential customers who have the same attributes as those who converted. Lastly, you can scrape data from Google to enrich your lead profiles and improve the accuracy of your predictive models.
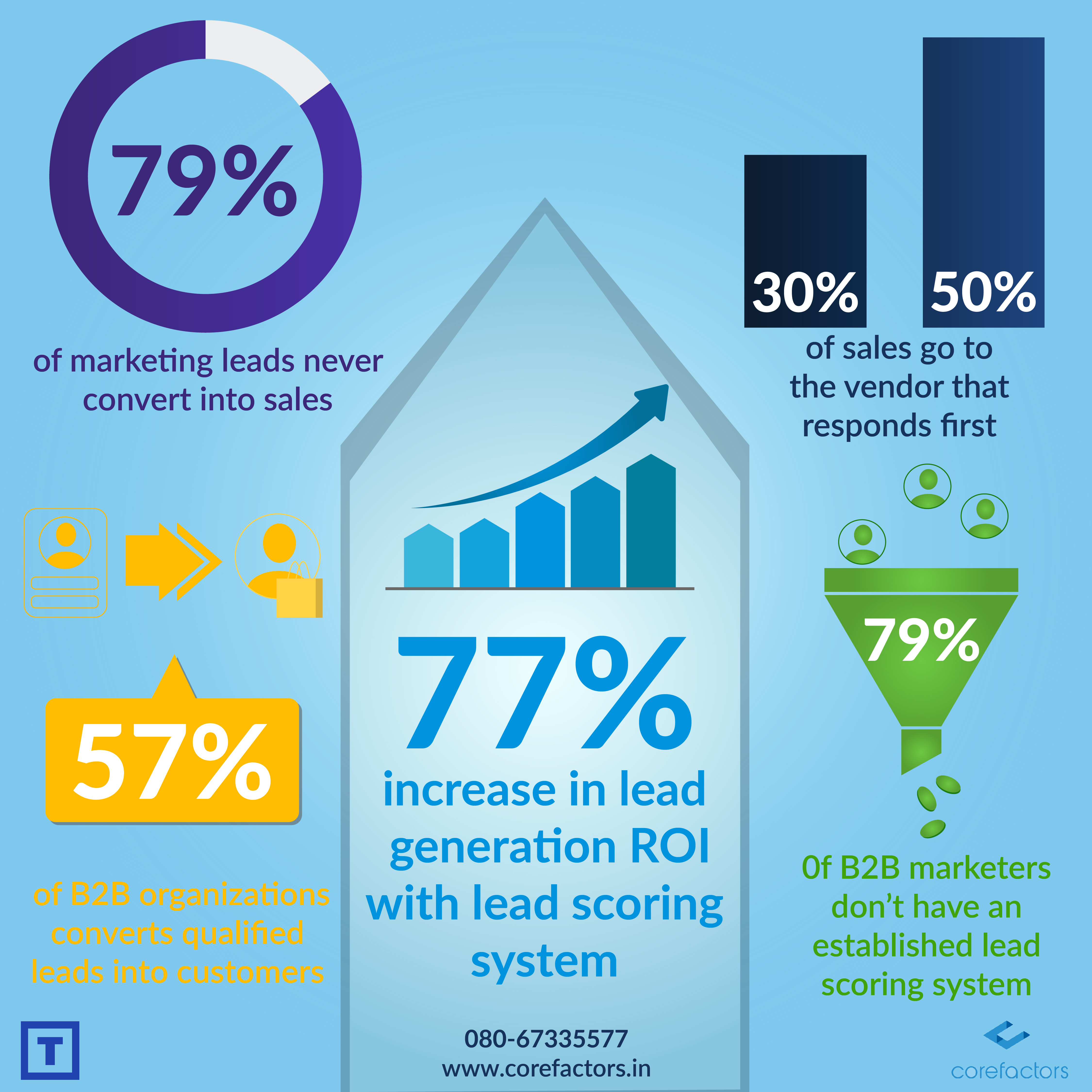
4 Benefits of Implementing a Lead Scoring Strategy
As you adopt lead scoring best practices, you will be able to reduce lead leakage to zero, convert more, add to the productivity of your sales team, and so on.
a) Reduced Lost Opportunities: As you start using a lead scoring system, your sales team will have a clear direction on which leads to run follow up for. When you use an award-winning lead management system like Teleduce, you will be able to nurture leads with a low lead score.
b) Improved Conversion Rate: When you follow up leads that have already engaged in some sort of activity on your website or with your product, you will be able to increase conversion by a significant extent.

c) Enhanced Productivity: With a lead scoring system in place, your sales team will not be wasting time speaking to leads who are not sales-ready yet. This helps you to direct your sales team’s energy to nurture the right prospects.
d) Increased ROI: When your sales team gets in touch with prioritized prospects, chances are high that those leads will convert. This has a direct impact on the ROI generated by your company.
With lead scoring CRM like Teleduce, your sales funnel becomes one of the strongest assets for your company. Your sales team will find it much easier to follow up leads with a higher score determined by the attributes you set.
There is a world full of sales opportunities waiting to be discovered. Let your sales team win big with the award-winning sales and marketing automation platform Teleduce.